Muscle
Tone: What is it?
As therapists, we are many times asked by parents
“What is muscle tone?” Generally when
parents are asking this, it is because their child likely has high muscle tone
or spasticity. However, muscle tone can
be normal, high or low. So let’s start
with what is normal.
In 1966,
Stolov, defined the tone in the muscle as "the resistance of the muscle to
passive elongation or stretching" (1).
In other
words, it is the state of muscle tension inside a muscle or muscle group
when it is at rest.
Normal
Muscle Tone
Normal
tone means that there is
the right amount of “tension” inside the muscle at rest, and that the muscle is
inherently able to contract on command – we can tell our biceps to contract to
pick up a cup. Do not confuse “tone” with “strength”. Tone is the tension in
the muscle, set by the muscle spindles and the alpha and gamma nerves
associated with them. Strength is the
more of the number of muscle fibers and the ability to contract as a group to
produce a force. Although the two can
are connected, one does not precipitate the other (ie: high tone does not mean
high strength)
Low
Muscle Tone
Low
tone means there is not
enough tension in the muscle when it is at rest. When looking at a child with
low muscle tone, the muscles will not be defined and may have a floppy
feel. In general, because of the low tension,
there is a lack of graded control of the muscle when it is being
used. Graded control means that
just the right amount of movement and effort is used for the specific task.
To use
the coffee example again, when you decide you want to have a sip of coffee,
there is not enough tension in your muscles at rest. So you use a bit extra
momentum, maybe by flinging your arm out! You bump the cup a bit, get your
fingers around the handle and then drag it back, but the cup is heavy, and you
use too much oomph at first (to overcome the lack of “tension” in your muscles)
with the result that the coffee sloshes out!
Children
with low tone may well battle to sit upright at a desk for any period of time,
and may slouch over like the child in this picture. Children with low tone will often lean against any surface they can - walls, chair backs, etc.
They may
also lack endurance for gross and fine motor activities and may struggle with
games that require coordinated, controlled movements.
It is
important to remember that muscle tone is on a continuum – you can have
normal muscle tone that is a bit on the low side or a bit on the high side.
The tone
of the muscles affects postural control and postural stability.
Postural control and postural stability give you the “background” control of
your body that is necessary for helping you to stay upright and to stabilize
you during movement.
Postural
stability needs to develop in 3 main areas:
•
Neck
muscles
A lack of
stability in these areas may have an impact on a child's Fine Motor and Gross Motor Skills.
High
Muscle Tone
High
tone means there is too
much tension in the muscle at rest. In other words, the muscle is tight and
tense even though it is not doing anything. A child with spastic cerebral palsy
has high tone, which causes the arms and legs to be tightly contorted. When the
arms and legs are not regularly stretched and moved through physical therapy,
then “contractures” may occur, which mean less and less range of movement is
possible.
In the everyday example I gave above, if you had increased tone,
you would have to concentrate very hard and expend a lot of effort overcoming
the tension in your biceps in order to stretch out your arm. You may well end
up moving your whole body towards the coffee, as the tension in your arm
muscles is too high to be overcome with ease. Your movements are also likely to
be jerky.
Spasticity
Spasticity (meaning to draw or tug) is involuntary,
velocity-dependent, increased muscle tone that results in resistance to
movement. The condition may occur secondary to a disorder or trauma, such as a
spinal cord injury (SCI), a brain injury, a tumor, a stroke, multiple sclerosis
(MS), or a peripheral nerve injury. The severity of spasticity can change over
time, in different situations, and even with emotion.
Although
many therapeutic and medical interventions can attenuate its effects,
spasticity can be severely debilitating. In spite of the fact that spasticity
may coexist with other conditions, it should not be confused with any of the
following:
• Rigidity - Involuntary, bidirectional,
non – velocity-dependent resistance to movement
• Clonus - Self-sustaining, oscillating
movements secondary to hypertonicity
• Dystonia - Involuntary, sustained
contractions resulting in twisting, abnormal postures
• Athetoid movement - Involuntary,
irregular, confluent writhing movements
• Chorea - Involuntary, abrupt, rapid,
irregular, and unsustained movements
• Ballisms - Involuntary flinging movements
of the limbs or body
• Tremor - Involuntary, rhythmic,
repetitive oscillations that are not self-sustaining
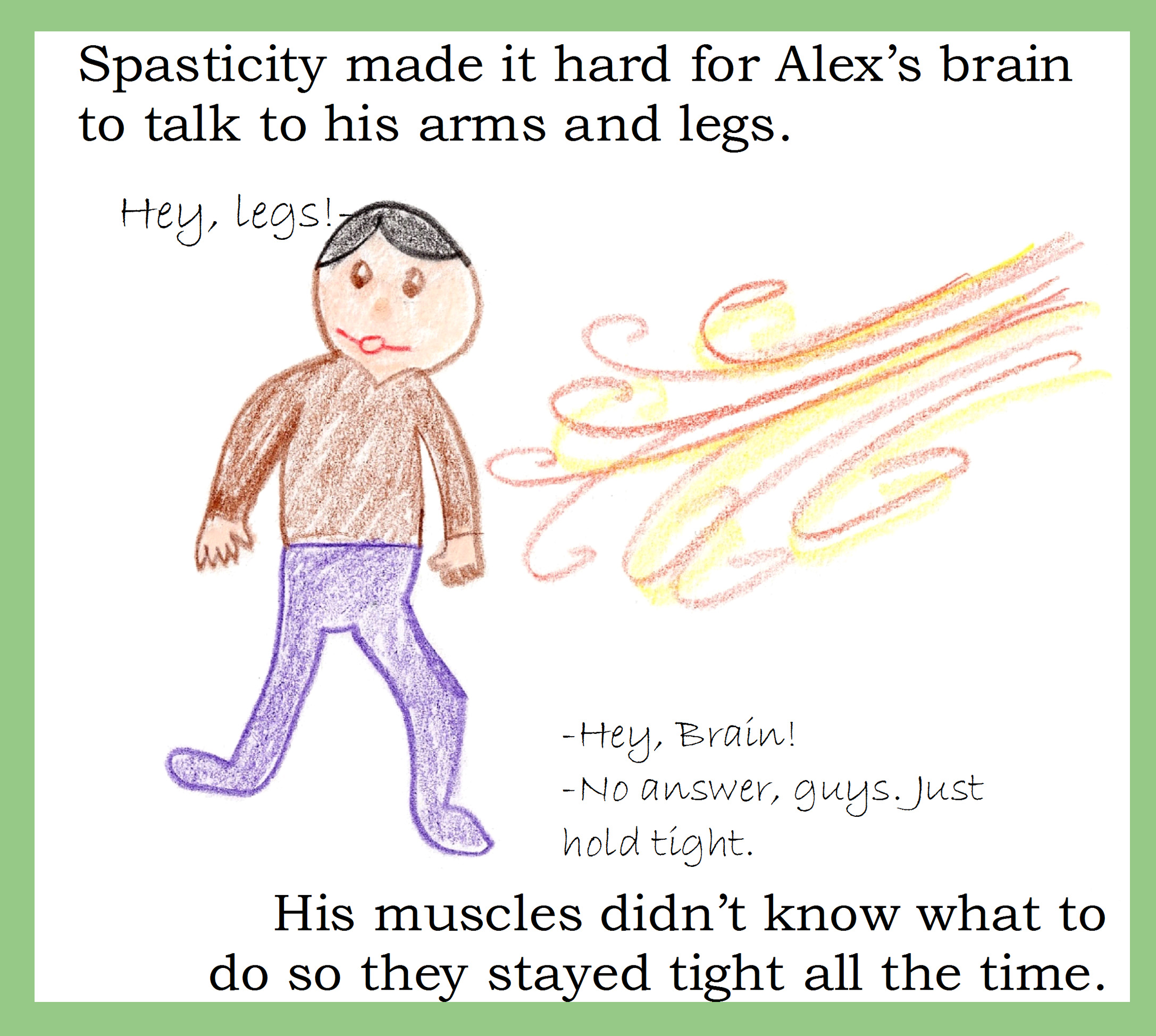
Saw this on the internet, thought it was an interesting way of talking about tone/spasticity
Frequency
Spasticity
is present to some degree in most patients with MS, SCI, cerebral palsy (CP),
and traumatic brain injury (TBI).
Advantages
of spasticity
Spasticity may sound like a completely detrimental
thing, but spasticity can actually help with function for many people.
Substitutes for strength, allowing
standing, walking, gripping (think tenodesis grip)
May improve circulation and prevent
deep venous thrombosis and edema
May reduce the risk of osteoporosis
– although must be careful with this, especially if person is non-weight
bearing
Morbidity/disadvantages
of spasticity
While spasticity does have some advantages, it is
still a very large consideration in the health, functionality, and quality of
life in most people.
Orthopedic deformity, such as hip
dislocation, contractures, or scoliosis
(surgery and botox can help here, but are not always successful)
Impairment of activities of daily
living (eg, dressing, bathing, toileting)
Impairment of mobility (eg,
inability to walk, roll, sit)
Skin breakdown secondary to
positioning difficulties and shearing pressure
Pain or abnormal sensory feedback
Poor weight gain secondary to high
caloric expenditure
Sleep disturbance
Depression secondary to lack of
functional independence
How to
Assess and Measure Spasticity
• Ashworth scale/Modified Ashworth - From
0-4 (normal to rigid tone)
Scoring (taken from Bohannon and Smith, 1987):
0: No increase in muscle tone
1: Slight increase in muscle tone, manifested by a catch and release or by minimal
resistance at the end of the range of motion when the affected part(s) is moved
in flexion or extension
1+: Slight increase in muscle tone, manifested by a catch, followed by minimal
resistance throughout the remainder (less than half) of the ROM
2: More marked increase in muscle tone through most of the ROM, but affected
part(s) easily moved
3: Considerable increase in muscle tone, passive movement difficult
4: Affected
part(s) rigid in flexion or extension
• Physician's rating scale - Gait pattern
and range of motion assessed
- a modified version of the
Physicians Rating Scale, known as the Observational Gait Scale (OGS)
- OGS was found to have acceptable
interrater and intrarater reliability for knee and foot position in mid-stance,
initial foot contact, and heel rise with weighted kappas (wk) ranging from 0.53
to 0.91 (intrarater) and 0.43 to 0.86 (interrater).
- Anna H Mackey, Glenis L Lobb,
Sharon E Walt and N Susan Stott (2003). Reliability and validity of the
Observational Gait Scale in children with spastic diplegia. Developmental
Medicine & Child Neurology, , pp 4-11.
• Penn Spasm Frequency Scale - From 0-4 (no
spasms to >10/h)
Composed of
2-parts; the first is a self report measure with items on 5-point scales
developed to augment clinical ratings of spasticity and provides a more
comprehensive assessment of spasticity.
Spasm
Frequency:
• 0 = No spasm
• 1 = Mild spasms induced by stimulation
• 2 = Infrequent full spasms occurring less
than once per hour
• 3 = Spasms occurring more than once per
hour
• 4 = Spasms occurring more than 10 times
per hour
Spasm
Severity:
1 = Mild
2 = Moderate
3 = Severe
If the
patient indicates no spasms in Part 1, then they do not proceed to Part 2. The
second component of the PSFS is a 3-point scale assessing the severity of
spasms.
Functional
scales such as the Functional Independence Measure or Gross Motor Function
Measure also may be valuable, although they do not measure spasticity directly.
Research-oriented
tools for measurement include the Tardieu scale, surface electromyography, isokinetic
dynamometry, the H reflex, the tonic vibration reflex, the F-wave response, the
flexor reflex response, and transcranial electrical/magnetic stimulation.[1]
*** rehabmeasures.org
has many great assessment
tools with explanations, directions, and norms
***
Below is a movie
for patient explanation of tone:
Resources/References
3.
http://cerebralpalsy.org/about-cerebral-palsy/symptoms/eight-clinical-signs-of-cerebral-palsy/#amt